Sanguis Labs Eradicates Cancer Cells in Blood During Surgery.
Advanced intraoperative solution for real-time detection and elimination of malignant cells in bloodstream. Trusted by top hematology and oncology experts.
Core Benefits
Elevating intraoperative cancer care
Sanguis Lab delivers a transformative solution for hematology and surgical teams, combining precision, speed, and scientific validation to improve outcomes for cancer patients.
- Real-time cancer cell detection
- Immediate identification of circulating cancer cells during surgery for rapid intervention.
- Targeted eradication technology
- Advanced cell targeting ensures precise elimination of malignant cells with minimal disruption.
- Seamless surgical workflow integration
- Designed for compatibility with existing surgical protocols and equipment.
- Backed by clinical studies
- Efficacy and safety validated by peer-reviewed research and clinical trials.
- Trusted technology created by Real Watcher Labs
- Created and tested by our private laboratories including complete AI automated sequencing of performance capabilities for cancer care.
Cancer Overview
- Cancer cells grow too rapidly Normal cells mature into distinct cell types. These different cell types have specific functions. For example, liver cells help your body metabolize proteins, fats and carbohydrates and help remove alcohol in your blood. Cancerous cells divide so quickly that they don’t have a chance to mature and become the specialized cells they set out to be.
- Cancer cells may influence normal cells. Cancer cells may actually affect the behavior of the normal cells, molecules and blood vessels near a tumor. For example, cancer cells may recruit normal cells to develop new blood vessels. These vessels keep the tumor alive—and give it a chance to grow—by providing it with oxygen and nutrients.
- Cancer cells ignore the body’s signals to stop dividing. Your body has a built-in process, called apoptosis or programmed cell death, that tells the body to get rid of cells it doesn’t need anymore. Normal cells are better at listening: They listen to the body’s cues and stop reproducing when enough cells are present.
- Cancer cells are invasive. Because cancer cells ignore the body’s signals to stop dividing, they start invading tissues nearby. If a tumor is benign, it may push up against neighboring tissues but won’t invade it. However, a malignant tumor invades tissue and can spread throughout the body.
- Cancer cells trick the immune system. You probably know your immune system helps you fight infection and disease. The immune system typically gets rid of abnormal or damaged cells. Cancer cells manage to evade this process, which allows tumors to grow.
Cancer Overview II
- Hematology specialists and surgical teams face challenges in real-time blood analysis for cancer cells. Advancements in technology like Sanguis Lab enable precise intraoperative detection and eradication of CTCs. Circulating tumor cells (CTCs) can evade standard detection methods.
- Metastatic spread remains a leading cause of cancer recurrence.
- Intraoperative blood analysis is critical for real-time decision making.
- Detection sensitivity determines patient outcomes and prognosis.
- Technological advances are enhancing intraoperative cancer management.
- Collaborative care between hematologists and surgeons is essential for optimal results. Integrating such solutions improves patient outcomes and advances the standard of cancer care.
Cancer Cells Are Different
- In shape, cancer cells often have an abnormal shape, both of the cell, and of the nucleus (the “brain” of the cell.) The nucleus appears both larger and darker than normal cells. Exhibit altered morphology and membrane markers compared to healthy blood cells.
- In activity, with the manipulation of the cellular processes by the cancer cells, a major temperature and pH change within the tumor microenvironment could easily effect them which is not usually the case in normal cells as they is a buffering system to protect the cells Demonstrate elevated proliferation rates and abnormal mitotic activity.
- In size, they found that normal cervical cells tend to have a brush layer consisting of a single average length - 2.4 micrometers (millionths of a meter) - while the cancerous cells have mostly two typical lengths - 2.6 and 0.45 micrometers. Show resistance to programmed cell death (apoptosis), complicating eradication.
- In temperature, the difference between cancerous and normal cells could be variable. Although there is this common concept that tumor cells tend to have slight increase. There is usually 1-2 degrees difference between cancerous and normal cells as usually quoted in research.Show resistance to programmed cell death (apoptosis), complicating eradication. Can evade immune surveillance, facilitating metastatic spread.
- Show resistance to programmed cell death (apoptosis), complicating eradication. Can evade immune surveillance, facilitating metastatic spread. Require advanced, intraoperative diagnostic technologies for precise detection and removal. • This is how we scan for, identify, and eliminate then in the blood stream.
What We Do
- • Make the world’s most accurate single cell in blood identification system which detect circulating tumor cells intraoperatively to enable real-time surgical decisions.
- Make the world’s most accurate single cell in blood eradication system that ensure high specificity and sensitivity for cancer cell detection in blood flow analysis during procedures.
- Integrate seamlessly with surgical workflow for minimal disruption to operating room protocols.
- Make the world’s first dual pass blood cleansing system which delivers rapid, actionable results that empower hematology and surgical teams.
- Support clinical decision-making through reliable, technology-driven analysis.
What We Do Not
- Make blood transfusion equipment we enhanse existing systems.
- Delay surgery with lengthy or complex procedures—our technology is designed for efficiency.
- Make blood plasma or oxygenation systems or Introduce experimental treatments outside established surgical protocols.
- Make surgical tools or monitoring equipment which could compromise patient safety by interfering with standard of care.
- Replace multidisciplinary team input in comprehensive cancer care.
- 2,000,000+
- Successful Simulations
- 99.6%
- Intraoperative Detection Accuracy
- 25+
- Patents Ready to File
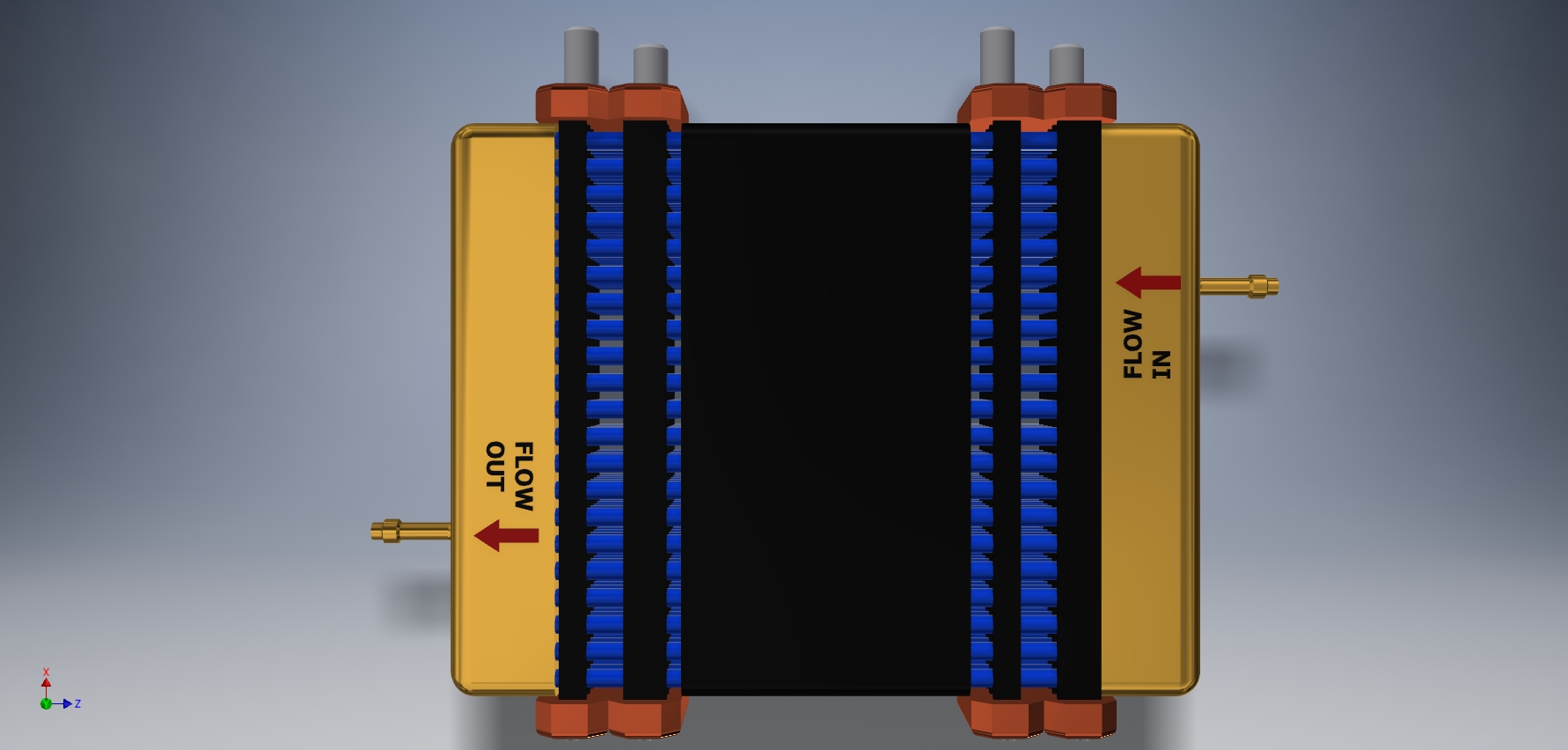
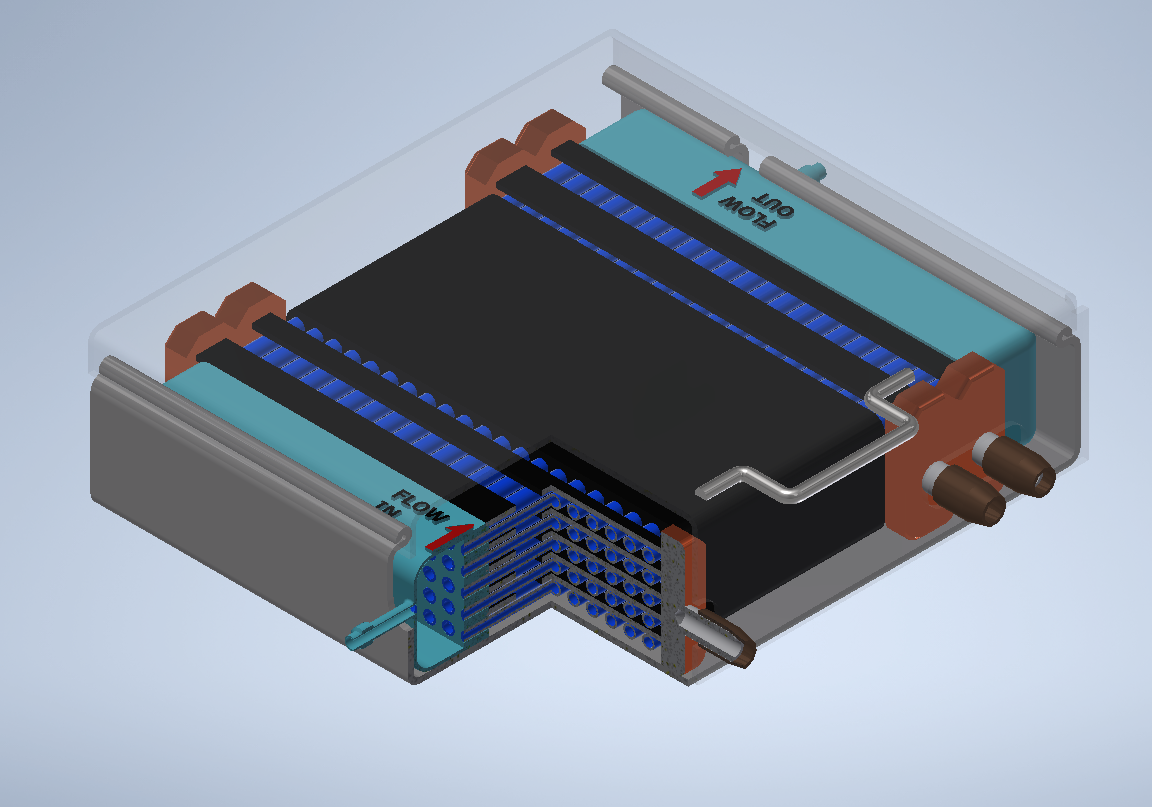
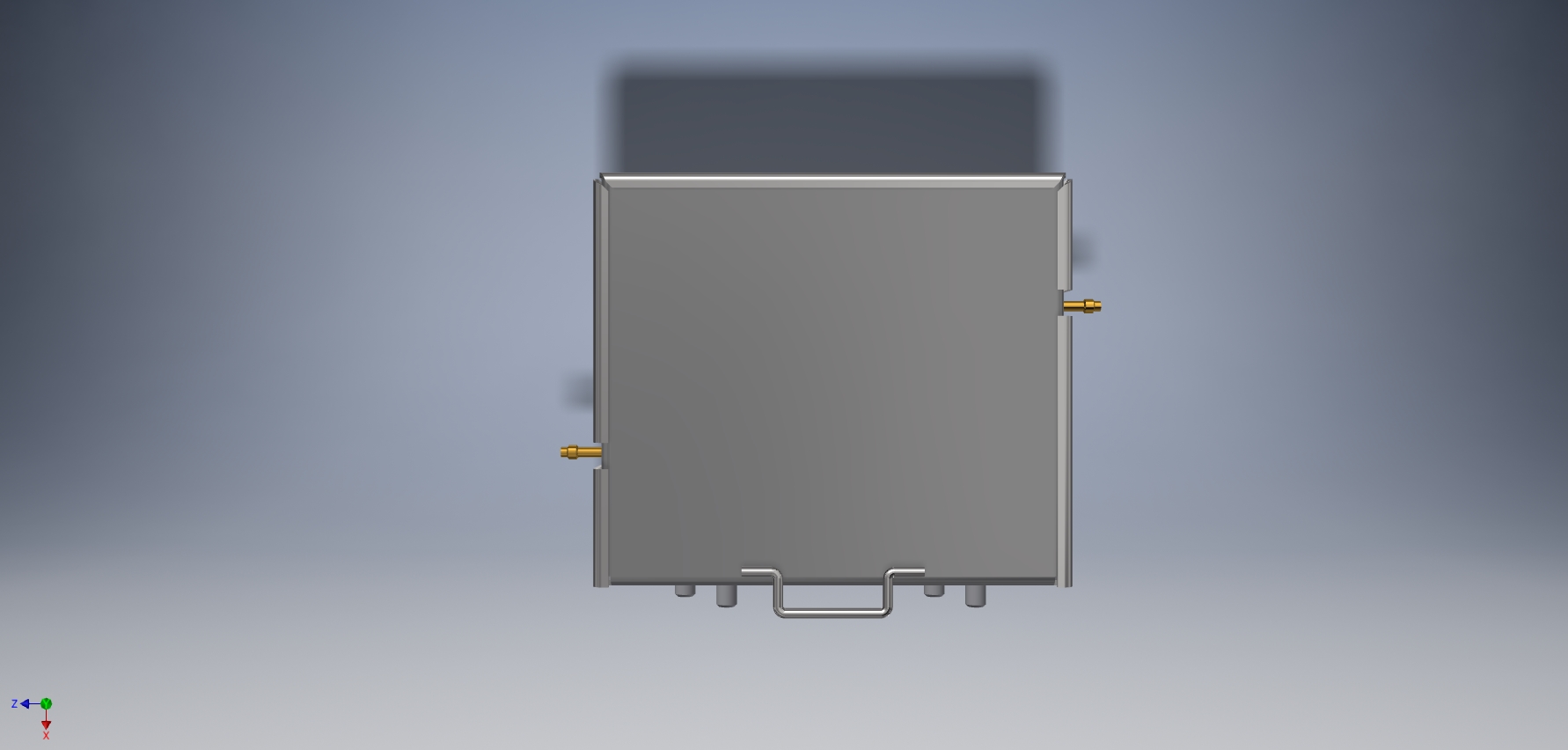
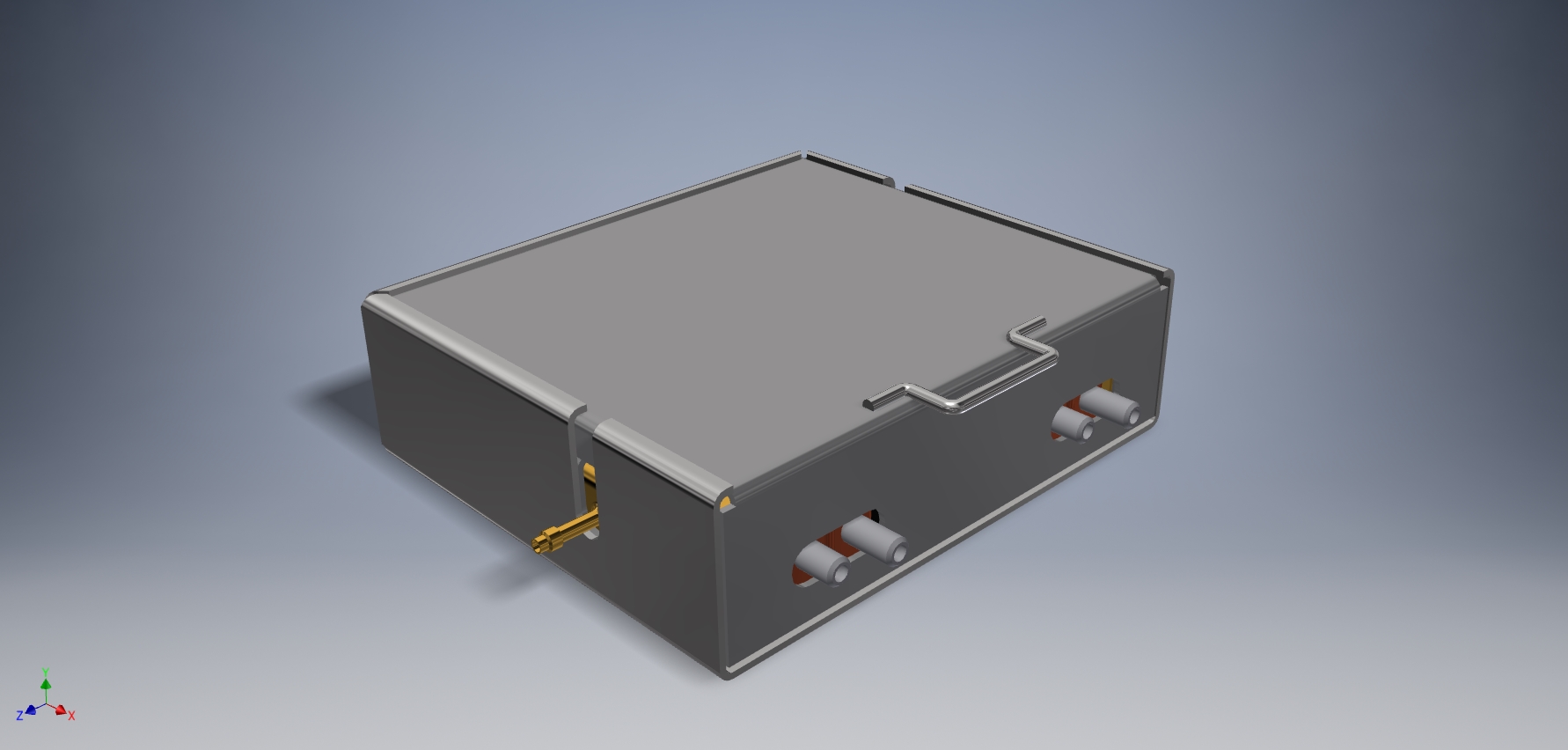
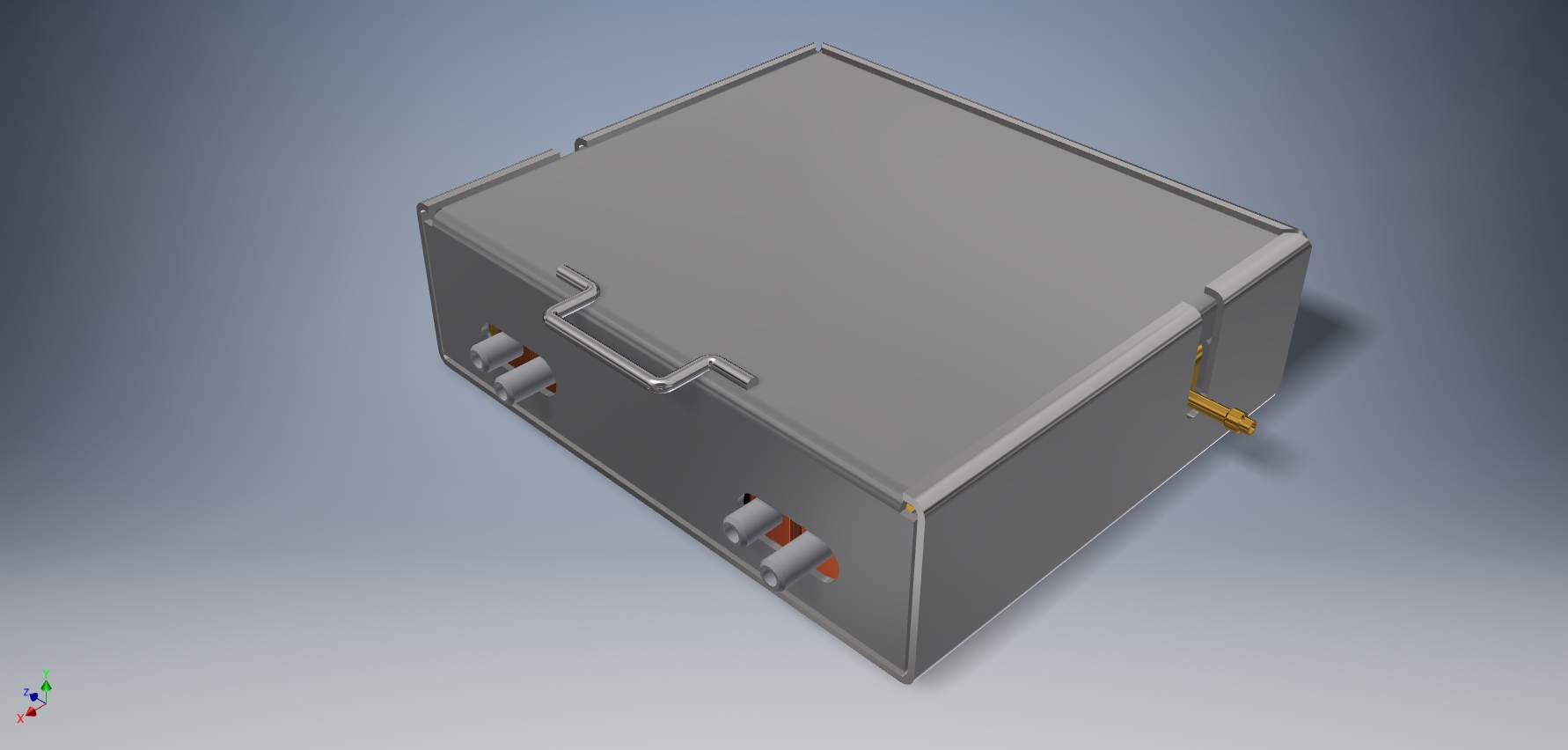
Engineering Images

Frequently Asked Questions
Have a question not listed here? Reach out to our support team by sending us an email and we'll respond promptly.
- How does Sanguis Lab detect cancer cells in blood during surgery?
- Sanguis Lab utilizes advanced flow cytometry and molecular marker recognition to identify and quantify circulating tumor cells in real time, providing immediate feedback to surgical teams.
- Is the technology safe for patients and compatible with operating room protocols?
- Yes. Sanguis Lab is designed for intraoperative use and operates with closed system protocols to ensure patient safety, sterility, and seamless integration within standard surgical workflows.
- Can Sanguis Lab be integrated with existing surgical equipment?
- Absolutely. The system features universal connectors and a modular platform, making it compatible with most contemporary surgical instruments and perfusion systems used in hematology and oncology procedures.
- What clinical results support the effectiveness of Sanguis Lab?
- Clinical studies have demonstrated a significant reduction in postoperative recurrence rates and improved detection accuracy when Sanguis Lab is employed during surgery. Detailed study data is available upon request.
- What training or certification is required for operating Sanguis Lab?
- Surgical and clinical staff receive comprehensive on-site training and ongoing support. Certification is provided following completion, ensuring optimal and safe utilization in all clinical settings.
Contact
+1 (754) 816-8507